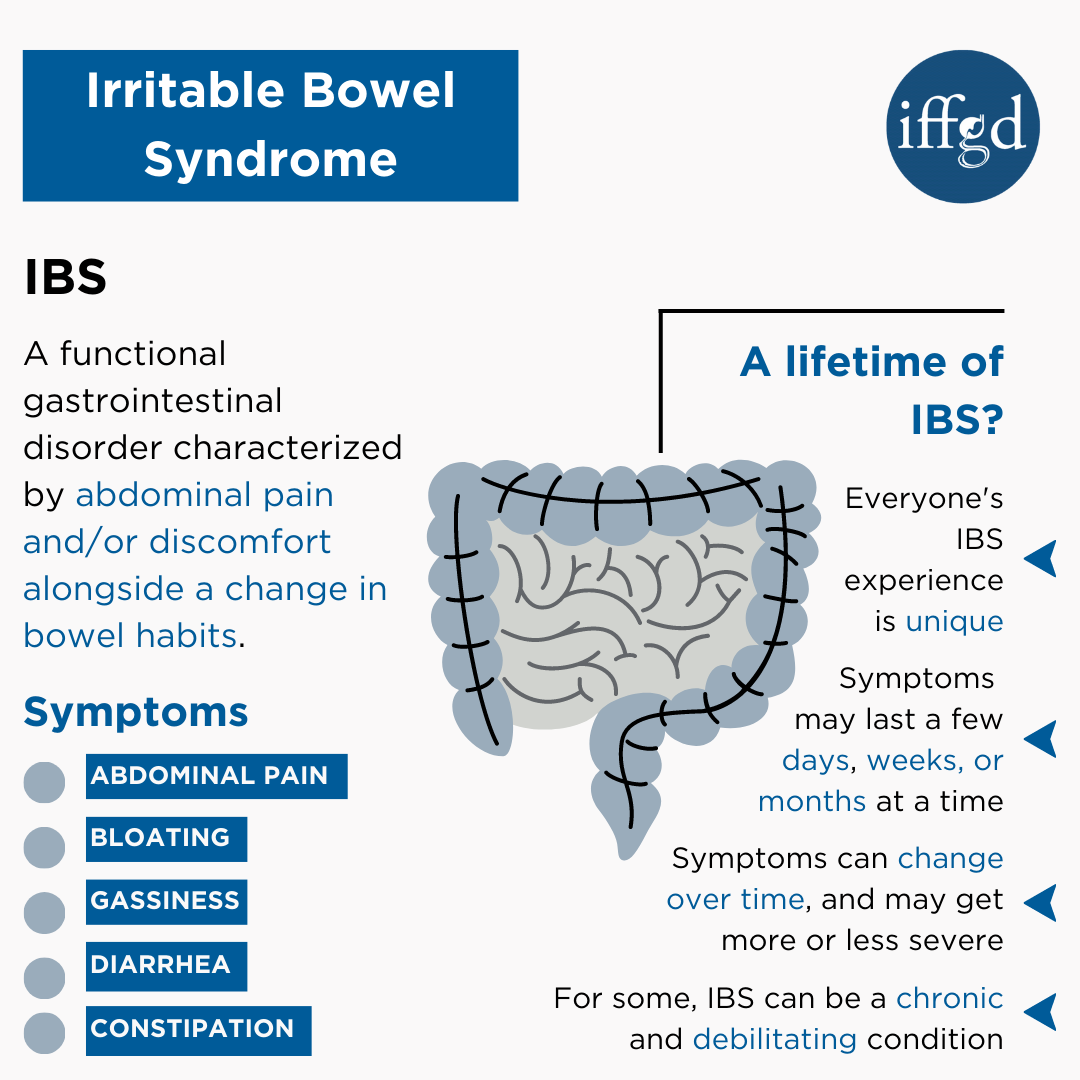
 Irritable bowel syndrome (IBS) is a gastrointestinal (GI) condition that causes recurrent attacks of abdominal pain or discomfort in association with bowel habits. This condition affects up to 5-10% of individuals worldwide and it can affect children and adults of both genders.
Irritable bowel syndrome (IBS) is a gastrointestinal (GI) condition that causes recurrent attacks of abdominal pain or discomfort in association with bowel habits. This condition affects up to 5-10% of individuals worldwide and it can affect children and adults of both genders.
Although irritable bowel syndrome does not shorten a person’s life span, it is associated with a large health care and economic burden. Studies have shown that IBS patients have an increased number of health care visits, diagnostic tests, and surgeries. IBS can also severely impact a person’s quality of life.
Understanding IBS
In IBS, the digestive system appears normal on routine tests. For this reason, it has been referred to as a functional gastrointestinal (GI) disorder. However, there is increasing evidence that the GI symptoms experienced in IBS may be caused by one of more of the following:
• Abnormalities in gut motility
• Improper functioning of the immune system (over or under active)
• changes in the bacteria that live in the gut (microbiota),
• minor increases in bowel inflammation (body responses to protect us from infection), and
• The central nervous system’s interpretation of painful signals coming from the gut.
These changes can alter the way the digestive system functions and how the brain senses things that are happening in the bowels. Sometimes IBS will develop after a person has a food poisoning or bowel infection (enteritis). More recently, it has been discovered that in some IBS patients there is a change in the way the brain controls the functions of the bowel, and also in how the bowel sends information back to the brain.
These disturbances can produce symptoms of abdominal pain or discomfort, bloating or a sense of gaseousness, and a change in bowel habits (diarrhea and/or constipation).
Is IBS inherited?
There are several studies showing that children of mothers with IBS are slightly more likely to be diagnosed with IBS. Also, siblings of IBS patients are more likely to have the condition as well. These studies suggest that certain genes play a role in IBS. This research is ongoing and hopefully lead to the development of a diagnostic test for IBS in the future.
A lifetime of IBS?
Each person’s illness experience with IBS is unique. Some can have symptoms a few days a month while others may have daily symptoms for weeks or months at a time. It is very common for the symptoms to change as well as the subgroup (IBS-D, IBS-C or IBS-M) and severity to change.
IBS is often a chronic disease or illness that has ongoing symptoms and lasts a long time, typically many years of life-long. Many IBS patients will experience symptoms their whole life. One exception is for individuals who developed IBS after food poisoning or post-infectious IBS. More than half of post-infectious IBS patients will gradually get better over time. Some will completely recover.
IBS vs. IBD
Irritable bowel syndrome (IBS) is a separate condition from inflammatory bowel disease (IBD).
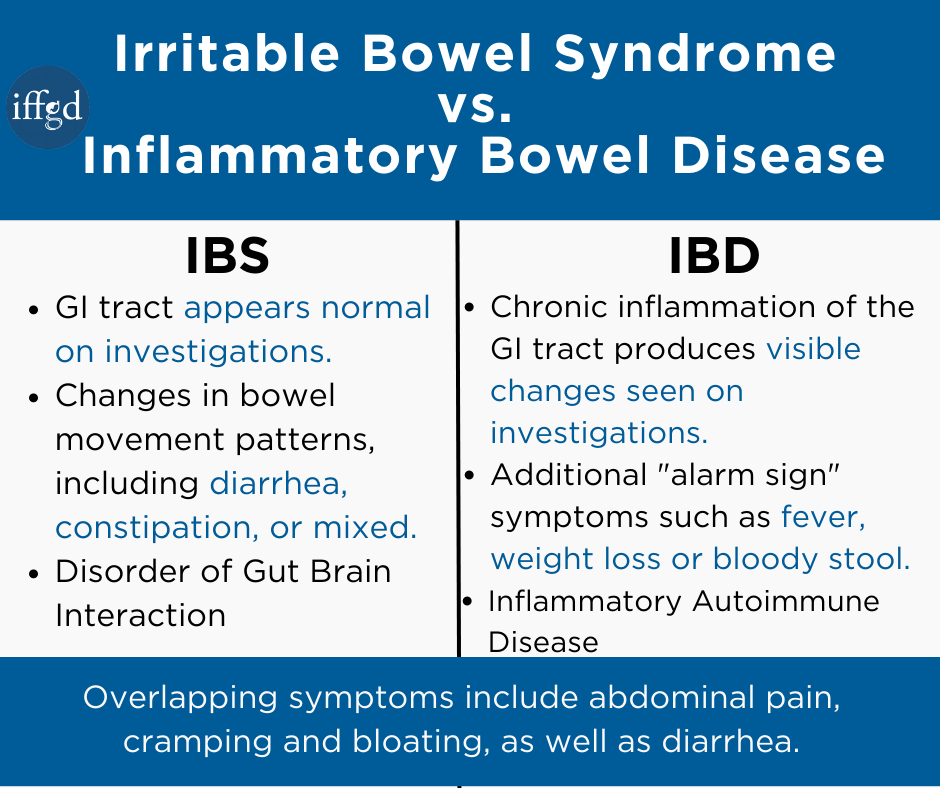
Inflammatory bowel disease (IBD) is a term for two conditions (Crohn’s disease and ulcerative colitis) that are characterized by chronic inflammation of the GI tract. Prolonged inflammation results in damage to the GI tract.
The two conditions sometimes get confused because of their similar acronym, and because of their similar symptoms.
Diarrhea, pain, bloating and cramping are symptoms of both IBD and IBS. However, IBD has other symptoms which set it apart from IBS. Fever, blood in stool and unintended weight loss, often referred to as “alarm signs”, should be discussed with a healthcare provider. IBD requires an entirely different treatment and monitoring plan than IBS. Those with IBS are not more likely to develop IBD.
When to be concerned that it’s more than IBS?
There is a collection of symptoms that healthcare providers use to make sure something other than IBS is not causing symptoms. “Concerning” or “alarm” features include:
- Blood in bowel movements – This blood can be bright red to black in color and may be in or around bowel movements.
- Low blood counts (anemia) – This is determined by blood work or lab tests ordered by a healthcare provider.
- New onset of symptoms over the age of 50.
- Unintentional weight loss
- Diarrhea that wakes you up from sleep at night.
If any of these “concerning features” are present, the patient should seek an immediate evaluation by their healthcare provider. Additional tests may be recommended to help find any potential issues.
Speaking with a healthcare provider about IBS
Patients should let their healthcare provider know about any family history of GI conditions, especially colon cancer, celiac disease, or inflammatory bowel disease. Also, symptoms that change either over time or suddenly such as the type of pain, severity, or frequency should be discussed with a healthcare provider.
Learn more about talking with your physician about irritable bowel syndrome
Although there is currently no cure for IBS, there are ways to improve symptoms and feel better. Find out how on this site.
Popular Topics about IBS
- Facts About IBS
- IBS Symptoms
- IBS Treatment & Management
- Gut Bacteria and IBS
- Other Disorders May Have Similar Symptoms
- IBS Research Trials
Adapted from IFFGD publication #110 “What to Expect When You Have IBS?” by Greg Sayuk MD, MPH, Associate Professor of Medicine and Psychiatry, Washington University School of Medicine; Edited by: William D. Chey, MD, AGAF, FACG, FACP, RFF, Nostrant Collegiate Professor, University of Michigan, Ann Arbor, MI











